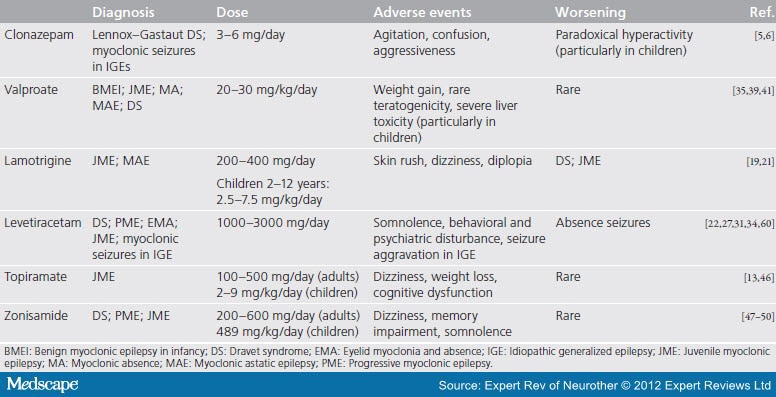
This article reviews data pertinent to evaluating the role of the newer AEDs, including felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, tiagabine, and topiramate, as monotherapy. Both new and earlier AEDs are generally equally effective in new-onset epilepsy. Therefore, patients with newly diagnosed epilepsy can begin treatment with a standard AED (carbamazepine, phenytoin, valproic acid/divalproex, phenobarbital) or with a newer agent . For children with newly diagnosed absence seizures, lamotrigine can be included in the options.
Seizure disorders become increasingly common after the age of 60 years and can have a significant impact on functional status. The goal of antiepileptic drug therapy is to control seizures but preserve quality of life. If possible, seizure control should be achieved with one agent given in the lowest effective dosage. Clinical response, rather than drug levels, should guide dosage changes. All antiepileptic drugs can cause dose-dependent sedation and cognitive impairment. Although the newer agents may have theoretical advantages over standard antiepileptic agents, higher cost may limit their use.
Drugs for first-line monotherapy of seizures in elderly patients include carbamazepine, valproic acid, oxcarbazepine, gabapentin, and lamotrigine. Neurocysticercosis is an infection of the brain with the tapeworm Taenia solium. On the Indian sub-continent, the majority of people suffering from neurocysticercosis only show one cyst in their brain and often present at clinics with epileptic seizures. There is still some debate on the best way to treat these cases to reduce the risk for seizure recurrence. The results show that ASM for 24 months compared to 6 months favors reduced seizure recurrence in patients whose cysts calcified post treatment. Concerning anti-inflammatory treatment, corticosteroids were also found to have beneficial effects on seizure reduction.
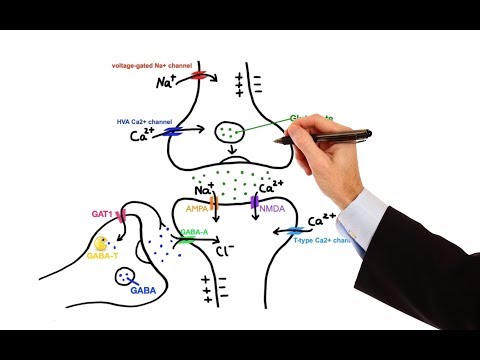
However, further high-quality randomized controlled trials with adequately long follow-up time are required for better evidence on best drug, dose and duration of ASM and corticosteroids for individuals with SEL NCC. The treatment initiation decision is dictated by the circumstances of a patient's seizure event . In 2015 the American Academy of Neurology and American Epilepsy Society released an evidence-based practice guideline for managing adult patients after a first unprovoked seizure. The risk of seizure recurrence is greater in the first 2 years; clinical variables such as a brain insult or EEG abnormality increase this risk. Seizure medications are often divided into narrow spectrum medications that are useful in treating focal onset seizures or broad spectrum that are useful in treating both focal onset and generalized onset seizures. Initiating treatment with a narrow spectrum agent in a patient with generalized onset seizures could lead to seizure worsening or pseudoexacerbation.
For adults 17 years of age and older with partial seizures, the recommended total daily dose of topiramate as adjunctive therapy is 200 to 400 mg/day in two divided doses. For adults with primary generalized tonic–clonic seizures, the recommended dose is 400 mg/day in two divided doses as adjunctive treatment. It is recommended that therapy be initiated at 25 to 50 mg/day, followed by titration to an effective dose in increments of 25 to 50 mg/week. Titrating the dose in increments of 25 mg/week may delay the time to reach an effective dose.
In studies of primary generalized tonic–clonic seizures, the initial titration rate was slower, and the assigned dose was reached at the end of eight weeks. When patients entered the double-blind phase, their absence seizures were fully controlled. Patients would exit the double-blind arm as soon as they were no longer seizure free. Therefore, the only patients exposed to placebo for 4 weeks were those who remained seizure free. Lamotrigine was significantly more effective than placebo, with 64% of patients receiving lamotrigine monotherapy free of absence seizures during the 4-week double-blind phase compared with 21% of placebo recipients. Lamotrigine was well tolerated, and no patient withdrew from the study because of adverse events.
The recommended initial dose is 15 mg/kg per day, increasing at one-week intervals by 5 to 10 mg/kg per day until seizures are controlled or until adverse effects preclude further increases. If the total daily dose exceeds 250 mg, the drug should be given in divided doses. A good correlation has not been established between daily dose, serum concentrations, and therapeutic effect. However, therapeutic valproate plasma concentrations for most patients with absence seizures range from 50 to 100 mcg/mL. After years of frustration, epilepsy researchers are shifting from targeting the seizures to seeking their cause, sometimes one patient at a time.
Much about the condition remains a mystery, including why antiseizure medications fail so many people, among them more than 1 million in the United States. Yet leaps in gene sequencing and better animal models are changing how scientists and doctors understand, study, and—sometimes—treat the disease. Generally, overall retention rates in these studies are low, and occurrence of adverse effects may be due to the high doses and rapid titration used. Several alternative study designs compare test medication with a suboptimal treatment, which may be a nontherapeutic dose of the same drug, a different drug, or a placebo.
This trial design compares the seizure frequency between the study drug and placebo, just as in other placebo-controlled trials. In general, it is advisable to "start low and go slow" with one agent. Results from the Veterans Affairs Cooperative Study20 on the effects of age on epilepsy and its treatment indicate that compared with younger adults, older adults appear to be more responsive to antiepileptic drug therapy.
However, they are also more likely to experience side effects at lower serum antiepileptic drug concentrations. Determination of the unbound drug concentration may be helpful when the clinical response appears inappropriate21 or side effects are prominent. Lamotrigine is indicated as an adjunctive therapy for partial seizures, primary generalized tonic–clonic seizures, and generalized seizures of Lennox–Gastaut syndrome in patients two years of age or older. This AED is also indicated for adults with partial seizures who are switching to monotherapy and are receiving carbamazepine , phenytoin , phenobarbital , primidone , or valproic acid (e.g., Depacon, Depakene) as the single AED.
The safety and efficacy of XCOPRI to treat partial-onset seizures was established in two randomized, double-blind, placebo-controlled studies that enrolled 655 adults. In these studies, patients had partial-onset seizures with or without secondary generalization for an average of approximately 24 years and median seizure frequency of 8.5 seizures per 28 days during an 8-week baseline period. During the trials, doses of 100, 200, and 400 milligrams daily of XCOPRI reduced the percent of seizures per 28 days compared with the placebo group.
Another study compared 8 antiepileptic drugs used in 20 randomized trials and reported that in patients with partial seizures, the results favored carbamazepine, oxcarbazepine, and lamotrigine. For generalized tonic-clonic seizures, the results favored valproate and phenytoin. At doses of 150 to 600 mg/day, pregabalin has been effective as an adjunctive therapy for adults with partial-onset seizures.
Both the efficacy and adverse-event profiles of pre-gabalin are dose-related. In general, it is recommended that patients begin with a total daily dose no greater than 150 mg . Based on individual patient response and tolerability, the dose may be increased to a maximum of 600 mg/day.
Further reductions of the concomitant AED dosage may be necessary in order to minimize adverse effects resulting from drug interactions. The felbamate dose is augmented in increments of 1,200 mg/day at weekly intervals to 3,600 mg/day. The duration of treatment is decided on an individual basis and in discussion with the physician. Some children have an epilepsy syndrome in which they will outgrow the tendency for seizures; thus anti-seizure medications can in some cases be discontinued under a physician's care . Unfortunately we know that some of the epilepsy syndromes have a life-long tendency and a poor chance of seizure-freedom thus medication discontinuation will usually not be recommended . Discontinuation of medications will be only advised in keeping with each individual's type of epilepsy and risk factors in mind.
Overall, studies have shown that up to one quarter to one third of people with epilepsy may have their anti-seizure medications discontinued after a period of seizure-freedom. There are over 20 different anti-seizure medications currently available and they differ in the way they work, the seizures they are best at treating, and the potential side effects. Thus physicians choose which medication to prescribe for the patients based on the type of epilepsy a person has and other factors such as age and gender. It is important for patients to know what the possible side effects are and to notify their physician if any side effects are experienced. The goal of treatment is always "No seizures, no side effects", however this may not be achieved in all patients.
Blood tests may be ordered for some anti-seizure medications to help with dosing decisions and to monitor for side effects. It is dangerous to stop medications or change doses on one's own without medical advice. Anti-seizure medications work best when they are taken at regular intervals and without any missed doses. Each year, 200,000 new cases of epilepsy are diagnosed, and 45,000 children younger than 15 years of age are affected.
Fifty percent of people with newly diagnosed epilepsy have generalized-onset seizures, which are more common in children younger than age 10. Afterward, more than 50% of all new patients with epilepsy have partial seizures. For women with epilepsy, pregnancy has historically been quite fraught. In generations past, epilepsy patients were discouraged from getting pregnant, as uncontrolled seizures can harm both mother and baby.
Older anti-seizure medications carry a high risk of physical birth defects and cognitive deficits in children exposed during pregnancy. Epilepsy Surgery– If a child has partial seizures which come from one area of the brain, surgery can sometimes be performed to remove the affected area. This type of surgery may "cure" epilepsy and the child may be able to stop all of their seizure medication over time. An extensive evaluation is done before offering this treatment. This option is not usually considered unless a child's seizures are not controlled by the first or second medication tried. The accepted principle is that one should begin with monotherapy.
All newer (second-generation) agents are acceptable choices and are likely just as effective as older agents. For adults, the initial clonazepam dose is divided into three doses. The dose may be titrated upward in increments of 0.5 to 1 mg every three days until seizures are adequately controlled or until side effects preclude any further increase. The maintenance dose must be individualized for each patient, depending upon the response. The maximum recommended daily dose is 20 mg.41 The use of multiple anticonvulsants may result in an increase of depressant adverse effects.
This consequence should be considered before clonazepam is added to an existing antiseizure regimen. Carbamazepine is indicated for use as an anticonvulsant drug. The recommendations regarding anti-inflammatory treatment are congruent with the American guidelines, and differ only in the grading (strong/moderate for the American guidelines). However, when considering the included studies all authors pointed out that it is crucial to differentiate between patients in whom cysts calcified and those in whom cysts resolved. Thus, when performing a sub-group analysis of patients whose cysts calcified in our study, anti-seizure medication of 24 months vs 6 months was found to be favoring reduced seizure recurrence, with a statistically significant result. In individuals with SEL NCC, symptomatic treatment such as anti-seizure medication for seizure control and anti-inflammatory drugs for the control of inflammation are commonly used.
However, the effectiveness of type, different dosage regimens and duration of ASM use remain controversial. There is also limited evidence to support the time point of ASM withdrawal [18–21]. Albeit not knowing their precise mechanism of action, corticosteroids are believed to have a beneficial effect on seizure outcome, because of their anti-inflammatory and anti-edema properties. Specific advantages of the newer AEDs include better tolerability, predictable kinetics, and broad-spectrum efficacy or well-defined spectrum of efficacy.
Furthermore, many of these studies employed flexible dose-titration schedules, allowing investigators to adjust doses. The most common side effect of seizure medications is feeling sleepy. When first starting a medication or when the dose is increased some children may feel a little drowsy for the first few days. Most children adjust to the medication and are back to feeling normal within a week.
We often start with a very low dose of medicine and slowly increase the dose to help control the sleepy feeling. Sometimes we have to increase the dose more quickly if a child is having frequent seizures and sleepiness may be more of a problem for the child. New findings published in the New England Journal of Medicine reveal that the three drugs, levetiracetam, fosphenytoin, and valproate, are equally safe and effective in treating patients with this condition. The study was supported by the National Institute of Neurological Disorders and Stroke , part of the National Institutes of Health. In patients over age 60 with new-onset epilepsy, focal seizures are the most common presentation.17 Overall head-to-head efficacy and tolerability trials in this population are limited.
Often a symptomatic or structural etiology is identified including stroke, a neurodegenerative process, or a tumor. Age-related changes in metabolism, renal clearance, gastrointestinal absorption, and serum albumin concentration may make dose adjustments necessary. For patients over age 60, it is often recommended medication be started at a lower dose and titrated slowly. It is also advised to avoid agents that induce hepatic enzymes because hepatic-enzyme induction may worsen cardiovascular risk factors. A thorough investigation of possible medication interactions is necessary, as polypharmacy in this patient population is common.
Another important point to consider is the risk of hyponatremia with oxcarbazepine, carbamazepine, or eslicarbazepine use, especially in those using diuretics. Newer AEDs are more expensive than the older drugs; this is clearly a problem for some individuals who must pay for their own medications. Common older drugs include valproic acid, phenytoin, carbamazepine, primidone, ethosuximide, clonazepam, and phenobarbital. Newer agents are gabapentin, lamotrigine, topiramate, tiagabine, levetiracetam, zonisamide, oxcarbazepine, pregabalin, eslicarbazepine, vigabatrin, lacosamide, and rufinamide.
Felbamate, approved in 1993, is now rarely used because of its potential for serious adverse effects. The dose should be increased by no more than 0.25 to 0.5 mg every third day until a daily maintenance dose of 0.1 to 0.2 mg/kg of body weight has been reached—unless seizures are controlled or side effects preclude further increases. For partial-onset seizures in adults 16 years of age and older, the initial dose is 1,000 mg/day, given as 500 mg twice daily. Additional dosing increments may be given as 1,000 mg/day every two weeks to a maximum recommended daily dose of 3,000 mg. Doses higher than 3,000 mg/day have been used in open-label studies for periods of six months and longer.
There is no evidence that doses greater than 3,000 mg/day confer additional benefit. Singhi et al. included 133 children with focal seizures and single small enhancing CT lesions in their randomized controlled trial to receive either corticosteroids , albendazole or corticosteroids and albendazole for 28 days. Of the initial patients, 23 were lost to follow-up, leaving 38 patients in group S, 37 in group A and 35 in group SA.
After a follow up of 3 and 6 months, cysts had resolved in 52.6% and 76.3% , 59.5% and 75.7% , and 62.9% and 74.2% of patients upon CT examination, respectively. Seizure recurrence was observed in 23 patients while being treated with ASM of whom 36.8% were in group S, 13.5% in group A and 11.4% in group SA. After ASM withdrawal, seven children, three in group S and two in group A and SA presented with seizure recurrence. Thus the authors concluded that corticosteroids alone are not recommended for management of SEL NCC in children. Prakash et al. included 52 patients with new-onset seizures and a "single CT lesion of cysticercus" in their open-label, randomized controlled trial.
The patients were either treated intravenously with methylprednisolone for 5 days plus ASM or with ASM alone. Levetiracetam is used alone and along with other medications to control partial-onset seizures in adults, children, and infants 1 month of age or older. Levetiracetam is also used in combination with other medications to treat seizure in adults and children 12 years of age or older with juvenile myoclonic epilepsy. Levetiracetam is in a class of medications called anticonvulsants.
When treating epilepsy, there are many antiepileptic drugs . AED choice depends on many factors such as doctor/client experience, potential side effects, cost, ease of dosing, and how rapid an onset is needed. The most commonly used AEDs are phenobarbital, potassium bromide, zonisamide, and levetiracetam. These drugs may be used alone or in combination to achieve the best control. It is crucial for the client to be involved in selecting a medical therapy for their pet. The explanation for the relatively low percentage of recurrence in this study compared to that of the first study may be that the inclusion criteria in the later study were more stringent.



















No comments:
Post a Comment
Note: Only a member of this blog may post a comment.